“They Were Talking to Each Other, But Not to Me”: Understanding the Patient Experience During Hospital-to-SNF Transitions



Transitions in healthcare can be stressful, especially for older adults who are moving from the hospital to a skilled nursing facility (SNF) for rehabilitation and recovery. A recent study by researchers at UCSF, “‘They Were Talking to Each Other, But Not to Me’: Examining the Drivers of Patients’ Poor Experiences During the Transition From the Hospital to Skilled Nursing Facility,” sheds light on why these transitions often feel fragmented and unsatisfactory for patients and their families.
The findings offer important lessons for anyone seeking to improve care transitions—whether you’re a healthcare professional, a family caregiver, or simply planning for a loved one’s future needs.
The Growing Importance of Hospital-to-SNF Transitions
Every year, millions of Americans are discharged from hospitals to SNFs—facilities designed to provide short-term rehabilitation and medical care after a serious illness, injury, or surgery. The ultimate goal is to help individuals regain enough function and independence to safely return home—oftentimes with the support of family caregivers or professional in-home care. As the U.S. population ages, these transitions are becoming increasingly common and costly, making it more important than ever to ensure they are handled with care and attention to the patient’s needs.
Unfortunately, the transition from hospital to SNF is often described as fragmented, with poor communication and lack of coordination between hospital staff, SNF teams, patients, and caregivers. This can leave patients feeling unprepared, anxious, and disconnected from their own care plans.
What Did the Study Find?
The research team conducted in-depth interviews with patients, caregivers, and clinicians, as well as ethnographic observations of care activities in both hospital and SNF settings. The central theme that emerged was captured by a patient’s poignant observation: “They were talking to each other, but not to me.”
This phrase became the lens through which the researchers examined the drivers of poor patient and caregiver experiences during these transitions.
Key Drivers of Poor Experiences
The study identified several interconnected factors that contribute to negative experiences:
Lack of Direct Communication: Patients and caregivers often felt excluded from discussions about their care. Medical teams would talk to each other—sometimes even in front of the patient—but not directly involve the patient or their family in the conversation.
Insufficient Information: Many patients and caregivers reported that they did not receive clear explanations about what to expect during the transition, what the SNF admission would entail, or what the plan for recovery looked like. This led to confusion and uncertainty.
Pressure to Discharge: Hospitals often face pressure to discharge patients quickly to maintain throughput. This can result in rushed transitions, with less time for thorough discharge planning or patient education.
Complex Team Dynamics: Interdisciplinary care teams—while essential for managing complex needs—sometimes create confusion about who is responsible for communicating with the patient. Training and practice norms may inadvertently prioritize clinician-to-clinician communication over patient engagement.
Patient Vulnerability: The physical and emotional vulnerability of patients during this period makes clear, compassionate communication even more critical. When this is lacking, patients can feel powerless and anxious about their recovery.
The relationships between these factors are complex and dynamic. For example, a rushed discharge process can exacerbate communication breakdowns, while unclear team roles can make it even harder for patients to know whom to ask for information and difficult for seniors and their families to plan for what comes next.
Real-World Consequences
When patients and caregivers feel disconnected from the care team and uninformed about what’s happening, the consequences can be serious:
Increased anxiety and distress
Difficulty adjusting to the SNF environment
Poorer adherence to rehabilitation plans
Delayed recovery and, in some cases, unnecessary hospital readmissions
Why Does This Matter?
Understanding the root causes of poor experiences during hospital-to-SNF transitions is essential for improving care quality. The study’s findings highlight the need for:
Patient-Centered Communication: Ensuring that patients and families are active participants in discussions and decisions about their care.
Clear Information Sharing: Providing practical, understandable information about what to expect at every stage of the transition.
Team Coordination: Clarifying roles within the care team so that someone is always responsible for keeping the patient and their family informed.
These improvements are not just “nice to have”—they are essential for supporting safe, effective, and compassionate care for older adults during a vulnerable time.
What Can Families and Care Facilitators Do?
If you or a loved one is facing a transition from hospital to SNF, there are steps you can take to advocate for a better experience:
Ask Questions: Don’t hesitate to ask the care team to explain what’s happening, what the next steps are, and who your main point of contact will be at the SNF.
Request Written Information: Having a written summary of the care plan, medications, and rehabilitation goals can help you stay informed.
Involve a Trusted Advocate: If possible, have a family member or friend present during key conversations to help ask questions and remember important details. This is where a care manager or elder care coach, who understands the whole process, can play a highly valuable role.
Clarify Expectations: Ask about what to expect during the SNF stay, how long rehabilitation might take, and what the plan is for returning home.
Looking Ahead: Planning for What Comes After the SNF
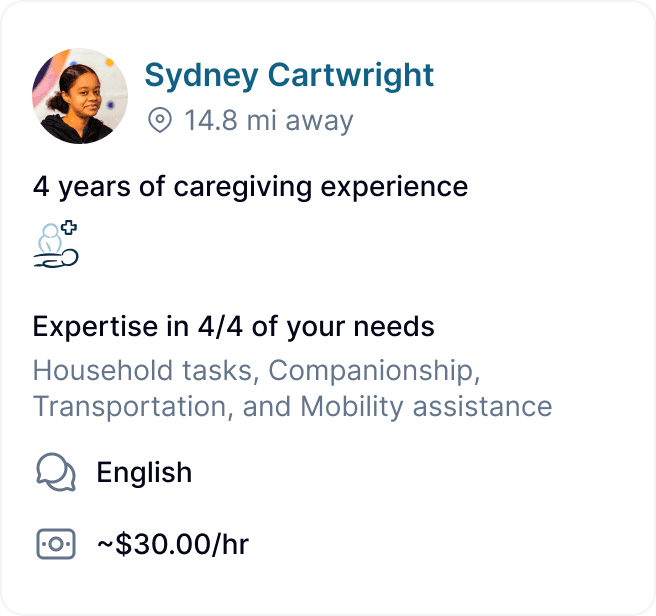
For many families, the journey doesn’t end after a SNF stay. Once a loved one is discharged, they may still need help with daily activities, medication management, or companionship at home. This is where home care becomes essential.
Services like Clara Home Care empower families to hire and manage vetted independent caregivers, providing continuity of support and peace of mind during the final stages of recovery and beyond.
Transitions in healthcare can be stressful, especially for older adults who are moving from the hospital to a skilled nursing facility (SNF) for rehabilitation and recovery. A recent study by researchers at UCSF, “‘They Were Talking to Each Other, But Not to Me’: Examining the Drivers of Patients’ Poor Experiences During the Transition From the Hospital to Skilled Nursing Facility,” sheds light on why these transitions often feel fragmented and unsatisfactory for patients and their families.
The findings offer important lessons for anyone seeking to improve care transitions—whether you’re a healthcare professional, a family caregiver, or simply planning for a loved one’s future needs.
The Growing Importance of Hospital-to-SNF Transitions
Every year, millions of Americans are discharged from hospitals to SNFs—facilities designed to provide short-term rehabilitation and medical care after a serious illness, injury, or surgery. The ultimate goal is to help individuals regain enough function and independence to safely return home—oftentimes with the support of family caregivers or professional in-home care. As the U.S. population ages, these transitions are becoming increasingly common and costly, making it more important than ever to ensure they are handled with care and attention to the patient’s needs.
Unfortunately, the transition from hospital to SNF is often described as fragmented, with poor communication and lack of coordination between hospital staff, SNF teams, patients, and caregivers. This can leave patients feeling unprepared, anxious, and disconnected from their own care plans.
What Did the Study Find?
The research team conducted in-depth interviews with patients, caregivers, and clinicians, as well as ethnographic observations of care activities in both hospital and SNF settings. The central theme that emerged was captured by a patient’s poignant observation: “They were talking to each other, but not to me.”
This phrase became the lens through which the researchers examined the drivers of poor patient and caregiver experiences during these transitions.
Key Drivers of Poor Experiences
The study identified several interconnected factors that contribute to negative experiences:
Lack of Direct Communication: Patients and caregivers often felt excluded from discussions about their care. Medical teams would talk to each other—sometimes even in front of the patient—but not directly involve the patient or their family in the conversation.
Insufficient Information: Many patients and caregivers reported that they did not receive clear explanations about what to expect during the transition, what the SNF admission would entail, or what the plan for recovery looked like. This led to confusion and uncertainty.
Pressure to Discharge: Hospitals often face pressure to discharge patients quickly to maintain throughput. This can result in rushed transitions, with less time for thorough discharge planning or patient education.
Complex Team Dynamics: Interdisciplinary care teams—while essential for managing complex needs—sometimes create confusion about who is responsible for communicating with the patient. Training and practice norms may inadvertently prioritize clinician-to-clinician communication over patient engagement.
Patient Vulnerability: The physical and emotional vulnerability of patients during this period makes clear, compassionate communication even more critical. When this is lacking, patients can feel powerless and anxious about their recovery.
The relationships between these factors are complex and dynamic. For example, a rushed discharge process can exacerbate communication breakdowns, while unclear team roles can make it even harder for patients to know whom to ask for information and difficult for seniors and their families to plan for what comes next.
Real-World Consequences
When patients and caregivers feel disconnected from the care team and uninformed about what’s happening, the consequences can be serious:
Increased anxiety and distress
Difficulty adjusting to the SNF environment
Poorer adherence to rehabilitation plans
Delayed recovery and, in some cases, unnecessary hospital readmissions
Why Does This Matter?
Understanding the root causes of poor experiences during hospital-to-SNF transitions is essential for improving care quality. The study’s findings highlight the need for:
Patient-Centered Communication: Ensuring that patients and families are active participants in discussions and decisions about their care.
Clear Information Sharing: Providing practical, understandable information about what to expect at every stage of the transition.
Team Coordination: Clarifying roles within the care team so that someone is always responsible for keeping the patient and their family informed.
These improvements are not just “nice to have”—they are essential for supporting safe, effective, and compassionate care for older adults during a vulnerable time.
What Can Families and Care Facilitators Do?
If you or a loved one is facing a transition from hospital to SNF, there are steps you can take to advocate for a better experience:
Ask Questions: Don’t hesitate to ask the care team to explain what’s happening, what the next steps are, and who your main point of contact will be at the SNF.
Request Written Information: Having a written summary of the care plan, medications, and rehabilitation goals can help you stay informed.
Involve a Trusted Advocate: If possible, have a family member or friend present during key conversations to help ask questions and remember important details. This is where a care manager or elder care coach, who understands the whole process, can play a highly valuable role.
Clarify Expectations: Ask about what to expect during the SNF stay, how long rehabilitation might take, and what the plan is for returning home.
Looking Ahead: Planning for What Comes After the SNF
For many families, the journey doesn’t end after a SNF stay. Once a loved one is discharged, they may still need help with daily activities, medication management, or companionship at home. This is where home care becomes essential.
Services like Clara Home Care empower families to hire and manage vetted independent caregivers, providing continuity of support and peace of mind during the final stages of recovery and beyond.
Transitions in healthcare can be stressful, especially for older adults who are moving from the hospital to a skilled nursing facility (SNF) for rehabilitation and recovery. A recent study by researchers at UCSF, “‘They Were Talking to Each Other, But Not to Me’: Examining the Drivers of Patients’ Poor Experiences During the Transition From the Hospital to Skilled Nursing Facility,” sheds light on why these transitions often feel fragmented and unsatisfactory for patients and their families.
The findings offer important lessons for anyone seeking to improve care transitions—whether you’re a healthcare professional, a family caregiver, or simply planning for a loved one’s future needs.
The Growing Importance of Hospital-to-SNF Transitions
Every year, millions of Americans are discharged from hospitals to SNFs—facilities designed to provide short-term rehabilitation and medical care after a serious illness, injury, or surgery. The ultimate goal is to help individuals regain enough function and independence to safely return home—oftentimes with the support of family caregivers or professional in-home care. As the U.S. population ages, these transitions are becoming increasingly common and costly, making it more important than ever to ensure they are handled with care and attention to the patient’s needs.
Unfortunately, the transition from hospital to SNF is often described as fragmented, with poor communication and lack of coordination between hospital staff, SNF teams, patients, and caregivers. This can leave patients feeling unprepared, anxious, and disconnected from their own care plans.
What Did the Study Find?
The research team conducted in-depth interviews with patients, caregivers, and clinicians, as well as ethnographic observations of care activities in both hospital and SNF settings. The central theme that emerged was captured by a patient’s poignant observation: “They were talking to each other, but not to me.”
This phrase became the lens through which the researchers examined the drivers of poor patient and caregiver experiences during these transitions.
Key Drivers of Poor Experiences
The study identified several interconnected factors that contribute to negative experiences:
Lack of Direct Communication: Patients and caregivers often felt excluded from discussions about their care. Medical teams would talk to each other—sometimes even in front of the patient—but not directly involve the patient or their family in the conversation.
Insufficient Information: Many patients and caregivers reported that they did not receive clear explanations about what to expect during the transition, what the SNF admission would entail, or what the plan for recovery looked like. This led to confusion and uncertainty.
Pressure to Discharge: Hospitals often face pressure to discharge patients quickly to maintain throughput. This can result in rushed transitions, with less time for thorough discharge planning or patient education.
Complex Team Dynamics: Interdisciplinary care teams—while essential for managing complex needs—sometimes create confusion about who is responsible for communicating with the patient. Training and practice norms may inadvertently prioritize clinician-to-clinician communication over patient engagement.
Patient Vulnerability: The physical and emotional vulnerability of patients during this period makes clear, compassionate communication even more critical. When this is lacking, patients can feel powerless and anxious about their recovery.
The relationships between these factors are complex and dynamic. For example, a rushed discharge process can exacerbate communication breakdowns, while unclear team roles can make it even harder for patients to know whom to ask for information and difficult for seniors and their families to plan for what comes next.
Real-World Consequences
When patients and caregivers feel disconnected from the care team and uninformed about what’s happening, the consequences can be serious:
Increased anxiety and distress
Difficulty adjusting to the SNF environment
Poorer adherence to rehabilitation plans
Delayed recovery and, in some cases, unnecessary hospital readmissions
Why Does This Matter?
Understanding the root causes of poor experiences during hospital-to-SNF transitions is essential for improving care quality. The study’s findings highlight the need for:
Patient-Centered Communication: Ensuring that patients and families are active participants in discussions and decisions about their care.
Clear Information Sharing: Providing practical, understandable information about what to expect at every stage of the transition.
Team Coordination: Clarifying roles within the care team so that someone is always responsible for keeping the patient and their family informed.
These improvements are not just “nice to have”—they are essential for supporting safe, effective, and compassionate care for older adults during a vulnerable time.
What Can Families and Care Facilitators Do?
If you or a loved one is facing a transition from hospital to SNF, there are steps you can take to advocate for a better experience:
Ask Questions: Don’t hesitate to ask the care team to explain what’s happening, what the next steps are, and who your main point of contact will be at the SNF.
Request Written Information: Having a written summary of the care plan, medications, and rehabilitation goals can help you stay informed.
Involve a Trusted Advocate: If possible, have a family member or friend present during key conversations to help ask questions and remember important details. This is where a care manager or elder care coach, who understands the whole process, can play a highly valuable role.
Clarify Expectations: Ask about what to expect during the SNF stay, how long rehabilitation might take, and what the plan is for returning home.
Looking Ahead: Planning for What Comes After the SNF
For many families, the journey doesn’t end after a SNF stay. Once a loved one is discharged, they may still need help with daily activities, medication management, or companionship at home. This is where home care becomes essential.
Services like Clara Home Care empower families to hire and manage vetted independent caregivers, providing continuity of support and peace of mind during the final stages of recovery and beyond.
More about senior health
More about senior health


Warning Signs Of Vision Loss In Seniors—And What To Do Next
Clara Editorial Team


Talking About Therapy: How to Normalize Mental Health Support with Aging Parents



Lowrie Hilladakis
Stroke Awareness Month: Navigating Recovery After the Crisis
Clara Editorial Team
Digestive Health Tips for Seniors: Why It’s Often Overlooked
Clara Editorial Team
What Is A Care Manager?
Camille Christie
The Physical and Mental Health Benefits of Gardening for Seniors



Quynh Thi Pham, OTS


Stay Sharp, Stay Happy: Fun ways to keep our mind active as we age!
Neelam Dabholkar, MBA
Nutrition Tips for Seniors at Home



Jon Levinson
How In-Home Senior Care Supports Independence



Lowrie Hilladakis
Building a Support Network: How Families Can Strengthen Connections for Seniors



Vanessa Bustos
GEt started for free
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.

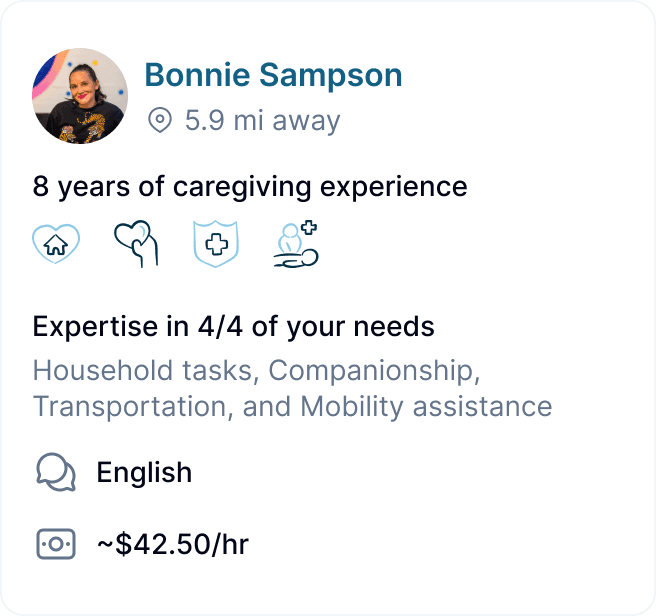
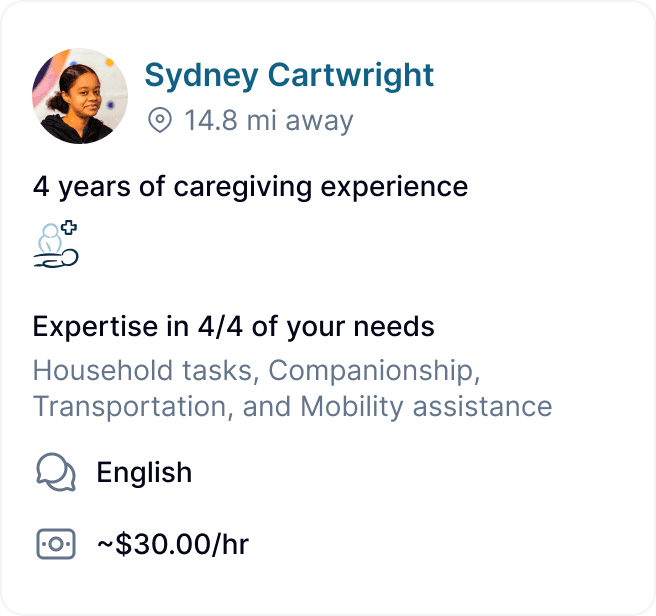
GEt started for free
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.

GEt started for free
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.

