How Policy Changes in Medicaid Could Your Family: What to Watch in 2025



As 2025 unfolds, Medicaid—the nation’s largest public health insurance program, covering one in five Americans—faces potential policy changes that could significantly impact families across the United States. Medicaid provides essential health and long-term care services for children, seniors, people with disabilities, and low-income adults—including in-home care support for the elderly. With Congress and the administration considering major reforms, understanding how these shifts could affect your family’s coverage, care access, and financial stability is more important than ever.
The Landscape: What’s on the Table for Medicaid in 2025?
Significant changes under discussion for 2025 include:
Federal funding cuts and financing reforms: Proposals include imposing per capita caps on federal Medicaid spending, reducing the federal match for Medicaid expansion under the Affordable Care Act (ACA), introducing or expanding work requirements, and lowering the minimum federal matching rate (FMAP) for states (1). There is also discussion of repealing incentives for states to expand Medicaid coverage.
Administrative and legislative actions: Even without new laws, the administration could implement changes through waivers, regulations, or guidance, affecting how states run their Medicaid programs.
If enacted, these changes could fundamentally alter Medicaid’s financing, shifting more responsibility-and risk-to states. States may be forced to cut the number of people covered, reduce benefits, or lower payment rates to providers.
How Could These Changes Affect Your Family?
1. Risk of Losing Coverage
Reductions in federal support for Medicaid expansion could prompt states to roll back eligibility or end expansion altogether. If the enhanced federal match for Medicaid expansion is eliminated, up to 20 million people could lose coverage, with total Medicaid enrollment dropping by nearly a quarter over ten years. The uninsured rate could increase by about 30%, reversing years of progress since the ACA (2).
Children are also at risk. Medicaid expansion has historically increased enrollment for both parents and children, improving health outcomes and financial stability. Scaling back coverage may leave children without access to preventive care, immunizations, and treatment for chronic condition.
2. Reduced Benefits and Provider Access
Funding cuts may force states to:
Reduce covered services (such as dental, vision, or mental health care)
Increase out-of-pocket costs for families
Lower payment rates to providers, making it harder to find doctors who accept Medicaid (3)
Families relying on home care services—like those provided through Medicaid-funded programs—could see reduced access, fewer hours of support, or be forced to seek more expensive institutional care if home-based options become unaffordable or unavailable.
3. Challenges for Long-Term Care and Home-Based Services
Medicaid is the primary payer for long-term services and supports (LTSS) in the United States, especially for seniors who need help with daily activities such as bathing, dressing, eating, and medication management. These services are not typically covered by private insurance.
As of 2024, Medicaid funds care for more than 60% of nursing home residents nationwide. Over 6 million people, mostly seniors and people with disabilities, rely on Medicaid for help with daily activities. If funding is reduced or eligibility tightened, families may face:
Longer waitlists for home-based care
Stricter eligibility criteria
Increased out-of-pocket costs or the need to provide unpaid care
4. State-by-State Variability
States may respond differently to federal policy changes. Some have “trigger laws” that automatically end Medicaid expansion if federal funding drops below a certain threshold, while others may require legislative action to reconsider expansion. This means your family’s access to Medicaid could depend heavily on where you live.
5. Impact on Special Populations
Families with members who have disabilities, chronic illnesses, or complex care needs are particularly vulnerable. Proposed reforms could allow states to reduce or eliminate mandatory benefits for children or redesign long-term care eligibility, potentially excluding middle-income families or those with moderate disabilities.
What Can Families Do?
Stay Informed and Engaged
Monitor state and federal policy developments; many changes will require legislative action and public input can influence outcomes.
Connect with advocacy organizations and your state’s Medicaid advisory groups to stay updated on proposed changes.
Plan for Potential Changes
Regularly review your family’s health coverage options and eligibility, especially if you anticipate changes in income or household composition.
Consider alternative support networks, such as local nonprofits or community health centers.
Advocate for Your Needs
Share your story with policymakers to highlight the real-world impact of Medicaid.
Participate in public comment periods on proposed state Medicaid changes or waivers.
Conclusion
Medicaid policy changes in 2025 could have far-reaching effects on families nationwide, impacting everything from basic health coverage to long-term and home-based care. While the details are still unfolding, staying informed, engaged, and connected to experienced providers will help families navigate uncertainty and advocate for the care they need.
The coming year will be pivotal for Medicaid and the millions who depend on it. Understanding the stakes and taking proactive steps can help safeguard your family’s health and well-being-no matter what changes lie ahead.
References
3. https://allianceforcareathome.org/the-alliance-opposes-medicaid-cuts-that-threaten-hcbs/
As 2025 unfolds, Medicaid—the nation’s largest public health insurance program, covering one in five Americans—faces potential policy changes that could significantly impact families across the United States. Medicaid provides essential health and long-term care services for children, seniors, people with disabilities, and low-income adults—including in-home care support for the elderly. With Congress and the administration considering major reforms, understanding how these shifts could affect your family’s coverage, care access, and financial stability is more important than ever.
The Landscape: What’s on the Table for Medicaid in 2025?
Significant changes under discussion for 2025 include:
Federal funding cuts and financing reforms: Proposals include imposing per capita caps on federal Medicaid spending, reducing the federal match for Medicaid expansion under the Affordable Care Act (ACA), introducing or expanding work requirements, and lowering the minimum federal matching rate (FMAP) for states (1). There is also discussion of repealing incentives for states to expand Medicaid coverage.
Administrative and legislative actions: Even without new laws, the administration could implement changes through waivers, regulations, or guidance, affecting how states run their Medicaid programs.
If enacted, these changes could fundamentally alter Medicaid’s financing, shifting more responsibility-and risk-to states. States may be forced to cut the number of people covered, reduce benefits, or lower payment rates to providers.
How Could These Changes Affect Your Family?
1. Risk of Losing Coverage
Reductions in federal support for Medicaid expansion could prompt states to roll back eligibility or end expansion altogether. If the enhanced federal match for Medicaid expansion is eliminated, up to 20 million people could lose coverage, with total Medicaid enrollment dropping by nearly a quarter over ten years. The uninsured rate could increase by about 30%, reversing years of progress since the ACA (2).
Children are also at risk. Medicaid expansion has historically increased enrollment for both parents and children, improving health outcomes and financial stability. Scaling back coverage may leave children without access to preventive care, immunizations, and treatment for chronic condition.
2. Reduced Benefits and Provider Access
Funding cuts may force states to:
Reduce covered services (such as dental, vision, or mental health care)
Increase out-of-pocket costs for families
Lower payment rates to providers, making it harder to find doctors who accept Medicaid (3)
Families relying on home care services—like those provided through Medicaid-funded programs—could see reduced access, fewer hours of support, or be forced to seek more expensive institutional care if home-based options become unaffordable or unavailable.
3. Challenges for Long-Term Care and Home-Based Services
Medicaid is the primary payer for long-term services and supports (LTSS) in the United States, especially for seniors who need help with daily activities such as bathing, dressing, eating, and medication management. These services are not typically covered by private insurance.
As of 2024, Medicaid funds care for more than 60% of nursing home residents nationwide. Over 6 million people, mostly seniors and people with disabilities, rely on Medicaid for help with daily activities. If funding is reduced or eligibility tightened, families may face:
Longer waitlists for home-based care
Stricter eligibility criteria
Increased out-of-pocket costs or the need to provide unpaid care
4. State-by-State Variability
States may respond differently to federal policy changes. Some have “trigger laws” that automatically end Medicaid expansion if federal funding drops below a certain threshold, while others may require legislative action to reconsider expansion. This means your family’s access to Medicaid could depend heavily on where you live.
5. Impact on Special Populations
Families with members who have disabilities, chronic illnesses, or complex care needs are particularly vulnerable. Proposed reforms could allow states to reduce or eliminate mandatory benefits for children or redesign long-term care eligibility, potentially excluding middle-income families or those with moderate disabilities.
What Can Families Do?
Stay Informed and Engaged
Monitor state and federal policy developments; many changes will require legislative action and public input can influence outcomes.
Connect with advocacy organizations and your state’s Medicaid advisory groups to stay updated on proposed changes.
Plan for Potential Changes
Regularly review your family’s health coverage options and eligibility, especially if you anticipate changes in income or household composition.
Consider alternative support networks, such as local nonprofits or community health centers.
Advocate for Your Needs
Share your story with policymakers to highlight the real-world impact of Medicaid.
Participate in public comment periods on proposed state Medicaid changes or waivers.
Conclusion
Medicaid policy changes in 2025 could have far-reaching effects on families nationwide, impacting everything from basic health coverage to long-term and home-based care. While the details are still unfolding, staying informed, engaged, and connected to experienced providers will help families navigate uncertainty and advocate for the care they need.
The coming year will be pivotal for Medicaid and the millions who depend on it. Understanding the stakes and taking proactive steps can help safeguard your family’s health and well-being-no matter what changes lie ahead.
References
3. https://allianceforcareathome.org/the-alliance-opposes-medicaid-cuts-that-threaten-hcbs/
As 2025 unfolds, Medicaid—the nation’s largest public health insurance program, covering one in five Americans—faces potential policy changes that could significantly impact families across the United States. Medicaid provides essential health and long-term care services for children, seniors, people with disabilities, and low-income adults—including in-home care support for the elderly. With Congress and the administration considering major reforms, understanding how these shifts could affect your family’s coverage, care access, and financial stability is more important than ever.
The Landscape: What’s on the Table for Medicaid in 2025?
Significant changes under discussion for 2025 include:
Federal funding cuts and financing reforms: Proposals include imposing per capita caps on federal Medicaid spending, reducing the federal match for Medicaid expansion under the Affordable Care Act (ACA), introducing or expanding work requirements, and lowering the minimum federal matching rate (FMAP) for states (1). There is also discussion of repealing incentives for states to expand Medicaid coverage.
Administrative and legislative actions: Even without new laws, the administration could implement changes through waivers, regulations, or guidance, affecting how states run their Medicaid programs.
If enacted, these changes could fundamentally alter Medicaid’s financing, shifting more responsibility-and risk-to states. States may be forced to cut the number of people covered, reduce benefits, or lower payment rates to providers.
How Could These Changes Affect Your Family?
1. Risk of Losing Coverage
Reductions in federal support for Medicaid expansion could prompt states to roll back eligibility or end expansion altogether. If the enhanced federal match for Medicaid expansion is eliminated, up to 20 million people could lose coverage, with total Medicaid enrollment dropping by nearly a quarter over ten years. The uninsured rate could increase by about 30%, reversing years of progress since the ACA (2).
Children are also at risk. Medicaid expansion has historically increased enrollment for both parents and children, improving health outcomes and financial stability. Scaling back coverage may leave children without access to preventive care, immunizations, and treatment for chronic condition.
2. Reduced Benefits and Provider Access
Funding cuts may force states to:
Reduce covered services (such as dental, vision, or mental health care)
Increase out-of-pocket costs for families
Lower payment rates to providers, making it harder to find doctors who accept Medicaid (3)
Families relying on home care services—like those provided through Medicaid-funded programs—could see reduced access, fewer hours of support, or be forced to seek more expensive institutional care if home-based options become unaffordable or unavailable.
3. Challenges for Long-Term Care and Home-Based Services
Medicaid is the primary payer for long-term services and supports (LTSS) in the United States, especially for seniors who need help with daily activities such as bathing, dressing, eating, and medication management. These services are not typically covered by private insurance.
As of 2024, Medicaid funds care for more than 60% of nursing home residents nationwide. Over 6 million people, mostly seniors and people with disabilities, rely on Medicaid for help with daily activities. If funding is reduced or eligibility tightened, families may face:
Longer waitlists for home-based care
Stricter eligibility criteria
Increased out-of-pocket costs or the need to provide unpaid care
4. State-by-State Variability
States may respond differently to federal policy changes. Some have “trigger laws” that automatically end Medicaid expansion if federal funding drops below a certain threshold, while others may require legislative action to reconsider expansion. This means your family’s access to Medicaid could depend heavily on where you live.
5. Impact on Special Populations
Families with members who have disabilities, chronic illnesses, or complex care needs are particularly vulnerable. Proposed reforms could allow states to reduce or eliminate mandatory benefits for children or redesign long-term care eligibility, potentially excluding middle-income families or those with moderate disabilities.
What Can Families Do?
Stay Informed and Engaged
Monitor state and federal policy developments; many changes will require legislative action and public input can influence outcomes.
Connect with advocacy organizations and your state’s Medicaid advisory groups to stay updated on proposed changes.
Plan for Potential Changes
Regularly review your family’s health coverage options and eligibility, especially if you anticipate changes in income or household composition.
Consider alternative support networks, such as local nonprofits or community health centers.
Advocate for Your Needs
Share your story with policymakers to highlight the real-world impact of Medicaid.
Participate in public comment periods on proposed state Medicaid changes or waivers.
Conclusion
Medicaid policy changes in 2025 could have far-reaching effects on families nationwide, impacting everything from basic health coverage to long-term and home-based care. While the details are still unfolding, staying informed, engaged, and connected to experienced providers will help families navigate uncertainty and advocate for the care they need.
The coming year will be pivotal for Medicaid and the millions who depend on it. Understanding the stakes and taking proactive steps can help safeguard your family’s health and well-being-no matter what changes lie ahead.
References
3. https://allianceforcareathome.org/the-alliance-opposes-medicaid-cuts-that-threaten-hcbs/
More about paying for care
More about paying for care


What is the cost of in-home care for stroke patients in California?
Clara Editorial Team


Holiday Pay: Should I Pay My Caregiver Overtime?



Jon Levinson


How Much Does Private Duty Home Care Cost?



Vanessa Bustos


What Is The Cost Of In-Home Dementia Care In California?



Ian Gillis


Tax Benefits and Deductions for Family Caregivers: Saving Money While Providing Care



Ian Gillis


Breaking Down Financial Barriers to Senior Care: Tips and Strategies



Jon Levinson


What is Long-Term Care Insurance? How It Can Support Your Loved Ones



Vanessa Bustos


How to Tackle Tough Financial Conversations with Your Aging Parents



Jon Levinson


Home Hospice Care Costs for Older Adults: What You Need to Know



Grady Shumway, MSW, LCSW


Does Medicare Cover In-Home Care for Seniors?



Ian Gillis
GEt started for free
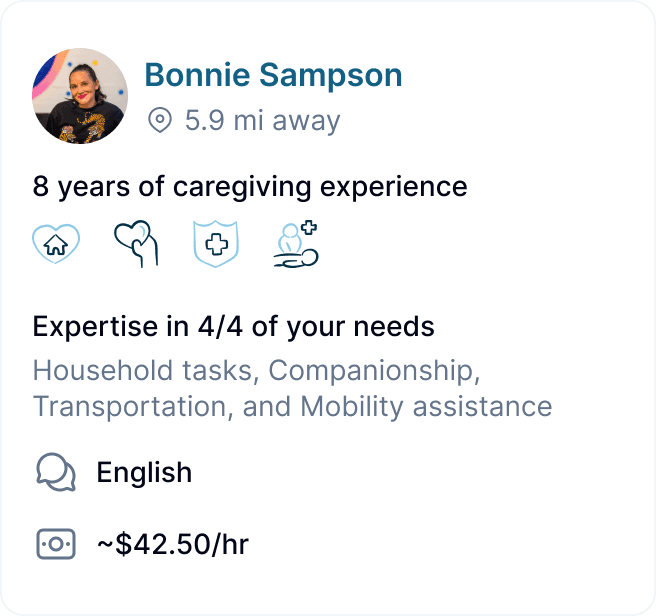
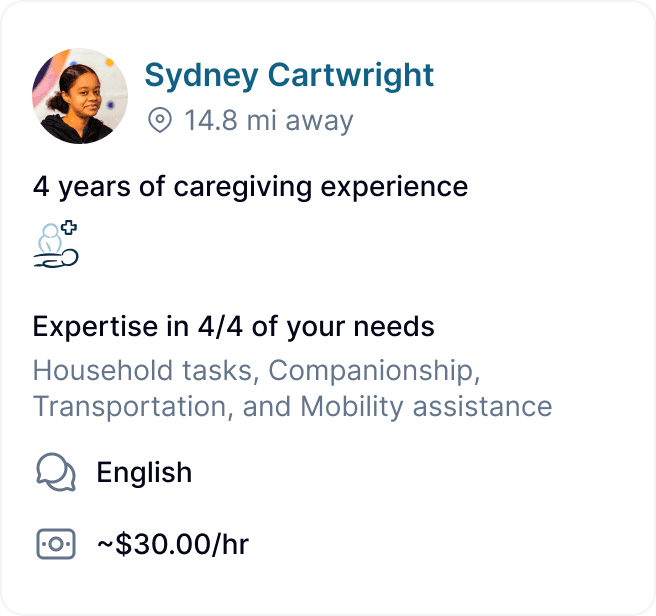
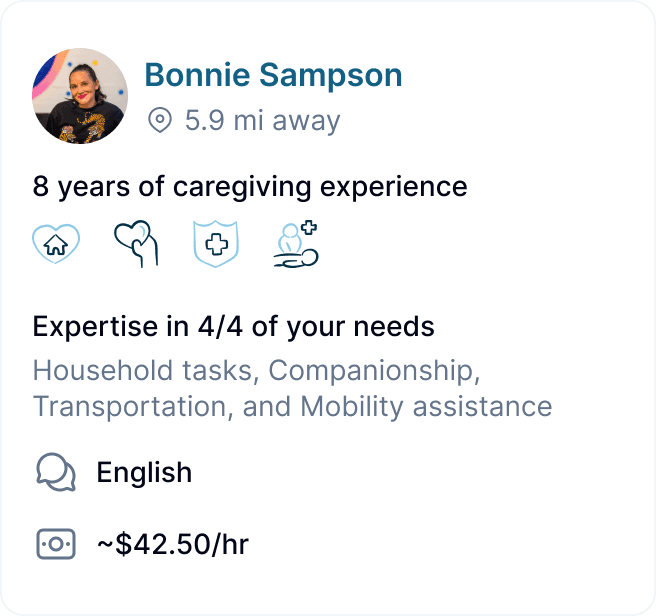
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.

GEt started for free
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.

GEt started for free
Better care starts with Clara.
Find, hire, and pay top-notch caregivers without the headache for a price that fits your budget.


